| Citation: | LI Jie, OU Shang-Kun, LI Wei, LIU Zu-Guo, PENG Qing-Hua. Physical Therapy Modalities of Western Medicine and Traditional Chinese Medicine for Meibomian Gland Dysfunction[J]. Digital Chinese Medicine, 2020, 3(4): 229-238. DOI: 10.1016/j.dcmed.2020.12.001 |
Meibomian gland dysfunction (MGD) is one of the most common diseases in ophthalmic practice. It is a prevalent disorder: the estimated pooled prevalence is 35.8%, with a higher prevalence of 46.2% - 69.3% in Asia and more than 80.0% of patients with dry eye disease (DED) having MGD in the United States and Europe [1, 2]. MGD occurrence increases with age, sleep disorders, contact lens wear and androgen deficiency [3]. In 2011, the International Workshop on MGD defined the condition as a chronic, diffuse abnormality of the meibomian gland, commonly characterized by terminal duct obstruction and/or qualitative or quantitative changes in the glandular secretion. These changes lead to alterations in the tear film lipid layer, with increased tear evaporation and osmolarity, symptoms of eye irritation, visual disturbance, clinically apparent inflammation and ocular surface diseases [4]. It is well accepted that MGD is the most common cause of evaporative DED [5].
Traditional Chinese medicine (TCM) ophthalmology has no corresponding disease named for MGD. Some descriptions of the ophthalmological diseases recorded in ancient books of TCM are similar to most of the symptoms and signs of MGD, such as “wind edge rotten eyes” in the Eye Collection of Standards of Diagnosis and Treatment, “fetid wind red rot” or “
The meibomian gland is sebaceous gland embedded in the tarsal plate of both the superior and inferior eyelids. The specific meibomian gland comprise meiocytes forming the acini that perform lipogenesis and mebium production [7-9]. The glandular secretion with the lipid and protein mixture maintains the osmolarity and stability, and prevents evaporation of the tear film [10, 11]. In the histopathological stage, because of the abnormal composition of mebium and the increase of viscosity, meibomian gland can undergo functional and structural changes, such as hyperkeratinization of the ductal epithelium in the meibomian gland [12, 13], leading to MGD. So, the ultimate goal of MGD management is to restore the function and structure of meibomian gland.
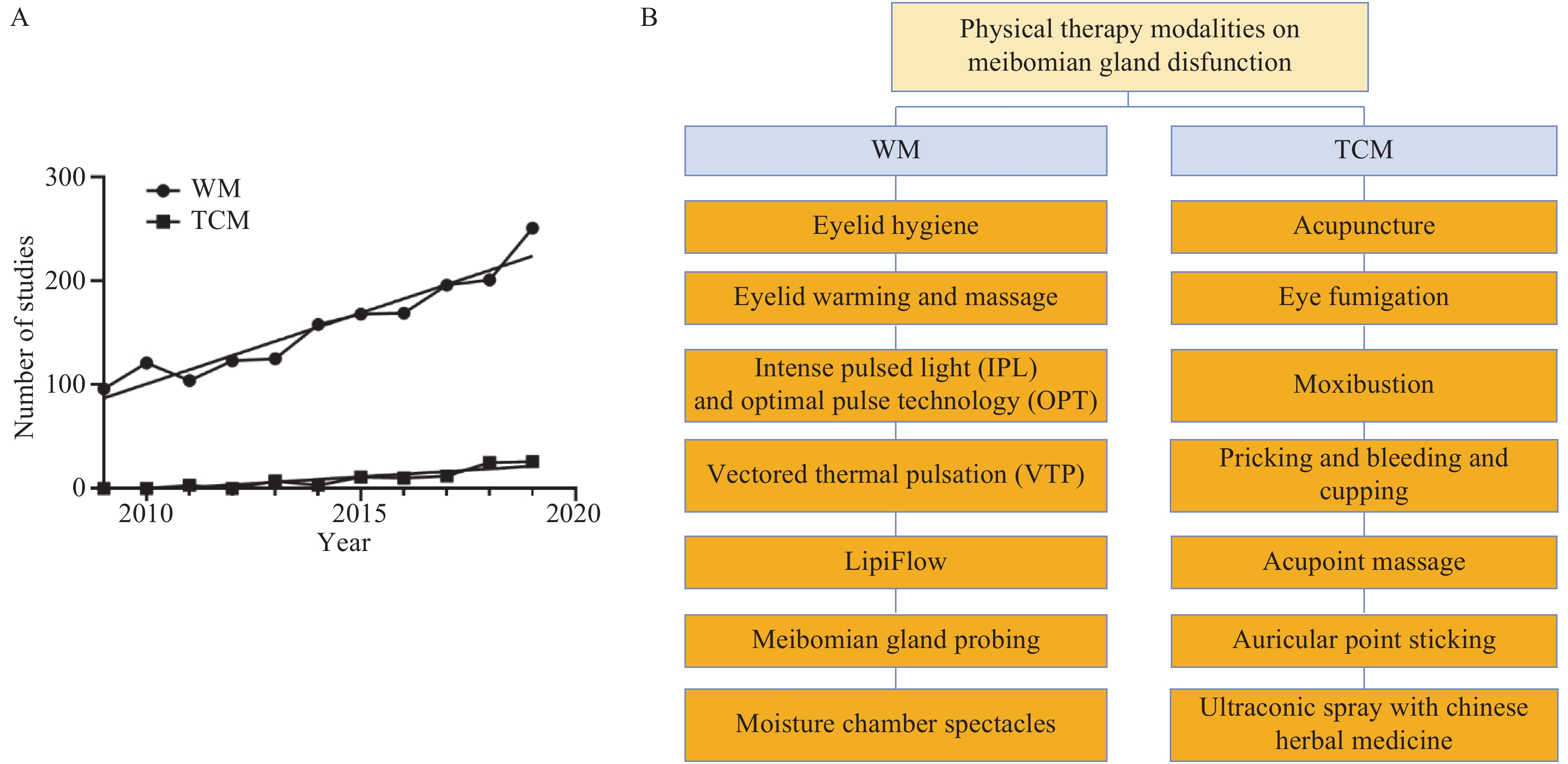
Many therapeutics have been proposed to treat MGD, including physiotherapy in western medicine (WM) and traditional Chinese medicine (TCM), artificial lubricants, anti-inflammatory agents, tetracycline, immunosuppressors and lubricant ointments. However, except for physiotherapy in WM and TCM, most of those strategies focus on alleviating symptoms or have severe side effects [14]. In contrast, physiotherapy focuses on restoring meibomian gland function and structure and has become one of the major forms of therapy (Figure 1A). This review summarized and evaluated the current studies on the physical therapy modalities in WM and TCM on MGD (Figure 1B).
The physical therapy modality in WM for MGD is a kind of non-pharmaceutical therapy. This includes a broad range of treatments, from low-tech solutions like eyelid hygiene, artificial eyelid warming and massage to high-tech solutions like automated eyelid warming and massage (LipiFlow® System), optimal pulsed light (OPT) therapy, intense pulsed light (IPL) therapy, etc. Each modality has special characteristics (Table 1), which are summarized below.
| Therapy | Medical devices | Treatment site | Therapeutic mechanism | Therapeutic effects |
| Eyelid hygiene | Wipes, pumps, gels, solutions, sprays and swabs containing anti-inflammatory, antimicrobial, anti-parasitic and antifungal ingredients | Eyelid margin | Cleanse the eyelid margin and lashes | ③④⑧[15] ⑦⑧[16] ①⑥[17] ①④⑧⑨[18] |
| Eyelid warming and massage | Artificial eyelid warming and massage devices | Both upper and lower external/inner eyelids | Artificial heating and evacuation of the gland contents | ④⑧⑪[19] ②④⑧[20] ②⑤⑪[21] |
| LipiFlow® System | Both upper and lower inner eyelids | Automated heating (42.5 °C) on both inner eyelid surfaces while pulsating pressure to evacuate the gland contents | ①⑥⑫[22] ①⑥⑦[23] ①②⑫[24] | |
| LipiFlow® Vectored Thermal Pulsation (VTP) System | Both upper and lower inner eyelids | Automated heat transfer and simultaneous evacuation of the gland contents while heating the glands to therapeutic levels (≥ 40 °C) | ①④⑥[25] ①④⑩[26] ①④⑧[27] | |
| IPL/OPT | IPL: IPL devices OPT: IPL devices (an optimal model for IPL) | The skin near the eyelids, four overlapping periocular zones under each eye, with the fifth pulse applied temporally adjacent to the lateral canthus | Selective thermal delivery to the meibomian glands and liquefication of the inspissated meibum | ④⑥⑧[28, 29] ⑤⑫[30] ①④[31] ②④⑧[32, 33] |
| ① Improved tear break-up time (TBUT); ② improved corneal or conjunctival fluorescein staining score; ③ improved lid margin lissamine green staining score; ④ improved meibum status or secretion; ⑤ improved eyelid margin and signs; ⑥ reduced ocular surface disease index (OSDI) score; ⑦improved meibomian gland atrophy; ⑧improvements in subjective symptoms; ⑨ improvement in meibomian orifice obstruction; ⑩ improved standard patient evaluation for eye dryness (SPEED) score; ⑪ improved visual analogue scale (VAS) score; ⑫ improved lipid layer thickness. | ||||
Eyelid hygiene plays an important role in decreasing the load of lipolytic bacteria and the amount of potentially toxic lipids on the ocular surface in products to induce tear film spoilage (e.g., free fatty acids), has become the first choice for the management of MGD and is still highly recommended [34]. Tear-free baby shampoos such as Johnson’s® No More Tears, combined with warm compresses, have become the customary treatment for MGD. A variety of lid scrubs are also commercially available and are effective for managing DED. However, an optimal cleaning solution is required as the above solutions contain amidoamine, 3-(dimethylamino) propylamine (MAPA), which is highly related to contact and eyelid dermatitis [35].
New products have been developed that contain substances that are anti-inflammatory, bactericidal and moisturizing. Several studies investigated advanced administration of eyelid hygiene, such as eyelid margin cleansing with ofloxacin ointment [36], eyelid hygiene treatment following cataract surgery [15], daily routine use of tap water and/or lid hygiene shampoo to cleanse the eyelid margin [16] in patients with MGD, and reported significantly improved in symptoms and signs.
Eyelid warming and massage remain the mainstay and most effective treatments for MGD nowadays. The application of warmth and massage to the eyelid margin can melt meibum plugging the terminal ducts and gland orifices and facilitate the delivery of meibum from the gland to the tear film [37]. Several commercial devices, such as the thermodynamic treatment device, MGDRx EyeBag and wet chamber warming goggles have been developed to retain heat more effectively [38, 39]. Repeated eyelid warming with a non-wet device can improve TBUT in normal individuals and also has beneficial effects on signs and symptoms of MGD [20, 21].
Various automated mechanical devices for eyelid massage have recently been developed based on conventional manual methods. One of them is the LipiFlow System™, which was approved by the Food and Drug Administration (FDA) as an automated alternative for liquefying meibum by thermal compression [22-24]. Another similar treatment is vectored thermal pulsation (VTP) therapy, which was designed to simultaneously evacuate the gland contents while heating the glands to therapeutic levels [25-27]. VTP can be applied to just the outer eyelids using an inflatable air bladder; while the LipiFlow can apply heat to both the inner and outer eyelid surfaces. Other reported mechanical devices include the fingers or auxiliary instruments such as meibomian gland squeezers, glass rods and local applications of medical apparatuses to evacuate stagnant meibum and improve meibomian gland function [40].
Several studies have indicated that eyelid warming and massage could improve symptoms and signs without serious adverse events in patients with MGD [22-27]. Besides, eyelid warming and massage combined with optimal antibacterial honey are effective adjunctive therapies for MGD [40, 41]. The effectiveness of meibomian gland massage combined with topical levofloxacin against ocular surface flora in patients before penetrating ocular surgery has been reported [42]. However, patients often feel discomfort such as mild pain during eyelid massage; with the pain more apparent during the first session compared to the following sessions. Conjunctival congestion and punctate hemorrhages of the lid margin may occur after eyelid massage [40]. Therefore, it is important to utilize reliable methods to provide optimal force during the procedure.
IPL is a broad-spectrum, non-coherent and polychromatic light source with a wavelength spectrum of 500 - 1200 nm produced by a high-output xenon lamp that can be filtered to allow the emission of a specific range of wavelengths [43]. IPL was optimized to allow a single light source (blue light) or blue light + IPL, termed optimal pulse technology (OPT), without increased adverse events. A growing number of physicians worldwide use IPL/OPT for the treatment of MGD and have reported improvements in symptoms, lipid layer grade, and meibomian gland secretion quality and productivity on the day after IPL therapy compared to those at baseline [44-46]. ALBIETZ et al. [44] reported that a combination of IPL and meibomian gland expression significantly improved dry eye symptoms and meibomian gland function. YIN et al. [47] compared the results of IPL therapy and eyelid hygiene, reported that both were equally effective in improving symptoms and meibomian gland function. Other studies indicated that IPL therapy was a safe therapy for long-term and regular use for MGD [29].
The mechanism by which IPL/OPT provides therapeutic effects to improve signs and symptoms on MGD remains vague. The proposed mechanisms include heat transfer, thrombosis of the vasculature around the meibomian gland, and decreased levels of inflammatory cytokines in the tears [48]. First some hypotheses propose that the heat produced by IPL/OPT could melt pathologically dysfunctional secretions and improve the obstructive orifices of the meibomian gland. Second, IPL/OPT significantly reduces levels of inflammatory cytokines such as interleukin (IL)-17A, IL-6 and prostaglandin E2 (PGE2), which are highly related to the clinical symptoms of DED induced by MGD. Third, IPL/OPT treatment can immediately reduce bacteria and mite load on the eyelid margin and their associated inflammation [49, 50]. However, the mechanism requires to be elucidated in future studies.
Other physical treatments in WM also have been reported for the treatment of MGD. Meibomian gland probing was proven to be a safe and effective method to relieve meibomian gland obstruction with symptom relief and tear film stabilization in patients with MGD [51, 52]. Wearing moisture chamber spectacles is a safe and promising alternative management for DED and MGD by improving ocular discomfort and tear film stability [53]. Three-dimensional (3D) printed personalized moisture chamber spectacles were an effective method to provide sufficiently high periocular humidity in a low-humidity environment in patients with MGD [54].
Physical therapy in TCM for MGD is based on the TCM syndrome differentiation, including the wind-heat attack of the exterior, damp-heat of the spleen and stomach, spleen and kidney yin deficiency, phlegm-damp obstruction of the eyelids, and Qi deficiencies of the spleen and stomach. Physical therapy is also called external therapy in TCM. The external treatment for MGD mainly includes acupuncture, eye fumigation and moxibustion MB. Different TCM syndrome differentiation in MGD use different external treatments according to its characteristics (Table 2).
| Therapy | Medical devices | Treatment site | Therapeutic mechanism | Therapeutic effects |
| Acupuncture | Needles for acupuncture | Jing Ming (BL1), Cuan Zhu (BL2), Yang Bai (GB14), Si Zhu Kong (TE23), Tai Yang (EX-HN5), Si Bai (ST2), He Gu (LI4), Tai Chong (LR3), Guang Ming (GB37), San Yin Jiao (SP6), Feng Chi (GB20), etc. | Promote meridian circulation, regulate Qi and blood | ①②④⑤[55] ①③[56] |
| Eye fumigation | Eye fumigation devices | Periorbital area and the ocular surface | Spread the external evil, nourish Yin and glory, dredge the meridians and collaterals, and unobstructed Qi and blood | ①③⑥[57] ①③[58] |
| Moxibustion | Moxa-moxibustion, thunder-fire moxibustion, walnut moxibustion, etc. | Periorbital area | dredging meridian, harmonizing Qi and blood, activating blood circulation and removing blood stasis, eliminating inflammation and analgesia | ①②③④[58] ①③[59] |
| ① Improved tear break-up time (TBUT); ② improved corneal or conjunctival fluorescein staining score; ③ increased tear production; ④ improved subjective symptoms; ⑤ improved eyelid margin and signs; ⑥ improved lipid layer thickness. | ||||
Acupuncture therapy is a promising strategy that promotes meridian circulation and regulates Qi and blood in patients with MGD patients. Acupuncture has been applied to select acupuncture sites for different syndromes in patients with MGD [60, 61]. The acupuncture points usually selected included Jing Ming (BL1), Cuan Zhu (BL2), Yang Bai (GB14), Si Zhu Kong (TE23), Tai Yang (EX-HN5), Si Bai (ST2), He Gu (LI4), Tai Chong (LR3), Guang Ming (GB37), San Yin Jiao (SP6), Feng Chi (GB20) and others. The reported course of treatment was three times a week for four weeks [55, 62-64].
Acupuncture shows effects by alleviating symptoms, increasing tear production, and improving TBUT and lipid deficiency in MGD patients. Several studies have observed the clinical effectiveness of acupuncture in the treatment of MGD, in which acupuncture applied at the periocular points was better at improving the palpebral margin score and increasing tear secretion, indicating a better therapeutic efficacy compared to WM [65, 66].
The potential molecular mechanisms of acupuncture may include the inhibition of the pro-inflammatory activities of interleukin-6 (IL-6), tumor necrosis factor (TNF)-α, and transfer growth factor (TGF)-β1 as well as increased lactoferrin level in tears to provide a bacteriostatic effect, thereby inhibiting inflammation of the ocular surface [67]. Additionally, acupuncture promotes the synthesis and secretion of mucins by goblet cells and the meibomian gland, increases the mucin content in tears, and restores tear film stability to restore the normal structure and function of the ocular surface [68, 69].
Eye fumigation therapy is believed to show effects by spreading the external evil, nourishing Yin and glory, dredging the meridians and collaterals, and improving unobstructed Qi and blood [70]. eye fumigation uses a medicine decoction to fumigate the eyes with its hot air transpiration. It has the dual effect of physical wet and hot compress and drug treatment. Reported studies applied eye fumigation for approximately 15 min each session, 1 - 3 times daily [71, 72].
In practice, eye fumigation usually uses fumigation or a fumigation combined with a washing. Clinically, a medicine tank with liquid is removed from the stove and the jar is then immediately covered with a thick sheet of paper or a thick paper cover with holes so that the hot air can fumigate the eyes. The temperature should be hot enough to endure without scalding as too low a temperature cannot achieve the purpose of eye fumigation. The liquid can be reheated. Studies in MGD patients have also reportedly used a heated steam kettle or an ultrasonic atomization inhaler for eye fumigation [70].
Several studies have reported the effectiveness of the combination of massage and eye fumigation on MGD. They believed that the clinical symptoms and signs in MGD patients were related to their cervical spondylosis, which caused increased pressure on the blood vessels and nerves, which affected tear circulation and quality to induce MGD. Thus, the combination of massage and eye fumigation could improve eye nutrition, promote tear secretion, and have a cleaning effect by clearing heat and providing detoxification [70, 73-75].
Moxibustion therapy dredges the meridian, harmonizes the Qi and blood, activates blood circulation and removes blood stasis, and eliminates inflammation and analgesia. Each course of treatment requires a daily Moxibustion session lasting approximately 30 min for 15 d for a total of two courses. After Moxibustion treatment, the symptoms, corneal fluorescence staining and TBUT are reportedly significantly improved; moreover, the operation was simple and easily accepted by children [76, 77].
Thunder-fire moxibustion has also shown a remarkable curative effect on MGD [78]. The combination of thunder-fire moxibustion with TCM improved meibomian gland function by nourishing the Yin on MGD patients [74, 79]. QIAN et al. [80] also reported that thunder-fire moxibustion with tobramycin dexamethasone eye drops was effective in treating MGD.
Other physical treatments of TCM, such as prick and bleeding and cupping, TCM hot package, and acupoint massage, could improve subjective symptoms, eyelid margin score and TBUT on MGD patients. The combination of TCM and acupoint massage reportedly eliminated eye fatigue, with a total effective rate of 93.3% [81]. Moreover, the combination of TCM ultrasonic cooling fog and moxibustion was also effective, with a total effective rate of 95.33% [82].
Physical therapy modalities are recommended and effective treatments for MGD. Physicotherapeutics of WM has been widely used in practice in the past three years, and many high-end clinical products have been developed. Therefore, it is well promoted in clinical practice. Physicotherapeutics of TCM has its advantages, but it is still relatively traditional, with few commercial benefits, and has not been widely promoted.
To enable MGD patients to receive appropriate physical treatment, standardization of MGD diagnosis and treatment is necessary. First, more studies are needed to assess tear film lipid layer thickness and alterations in the morphology and bacterial flora of the meibomian gland and the ocular surface, as well as tear osmolarity after physical treatments. Second, the mechanisms by which these physical strategies affect MGD requires clarification. Third, some modalities are expensive and not available in all clinics and the issue of cost may be a limitation for MGD patients. Last, the physiotherapy of TCM is based on clinical observations and lacks large samples and multi-center tests; therefore, it is necessary to continue to expand the research and strengthen future studies on these mechanisms.
We thank for the funding support from the Research and Innovation Project of Graduate Students in Hunan Province (No. CX20190538), the First-class Open Fund for Integrated Chinese and Western Medicine (No. 2018ZXYJH05), the Traditional Chinese Medicine First-Class Discipline Open Fund (No. 2018ZYX57), and the Construction Project of Hunan Engineering Technology Research Center for the Prevention and Treatment of Otorhinolaryngologic Diseases and Protection of Visual Function with Chinese Medicine (No. 2018YGC02).
| [1] |
HASSANZADEH S, VARMAGHANI M, ZAREI-GHANAVATI S, et al. Global prevalence of meibomian gland dysfunction: a systematic review and meta-analysis. Ocular Immunology and Inflammation, 2020. doi: 10.1080/09273948.2020.1755441.
|
| [2] |
YI TEO CH, ONG HS, LIU YC, et al. Meibomian gland dysfunction is the primary determinant of dry eye symptoms: analysis of 2 346 patients. Ocular Surface, 2020, 18(4): 604–612. doi: 10.1016/j.jtos.2020.06.008
|
| [3] |
LI S, NING K, ZHOU J, et al. Sleep deprivation disrupts the lacrimal system and induces dry eye disease. Experimental Molecular Medicine, 2018, 50(3): e451. doi: 10.1038/emm.2017.285
|
| [4] |
NGO W, GANN D, NICHOLS JJ. Impact of the 2011 international workshop on meibomian gland dysfunction on clinical trial attributes for meibomian gland dysfunction. Ocular Surface, 2020, 18(1): 27–30. doi: 10.1016/j.jtos.2019.10.003
|
| [5] |
AMANO S. Meibomian gland dysfunction: recent progress worldwide and in Japan. Investigative Ophthalmology Visual Science, 2018, 59(14): DES87–DES93. doi: 10.1167/iovs.17-23553
|
| [6] |
PENG QH. Ophthalmology of traditional Chinese medicine. Beijing: China Press of Traditional Chinese Medicine, 2016: 93-95, 119-121.
|
| [7] |
WILLCOX M, ARGüESO P, GEORGIEV GA, et al. TFOS DEWS II tear film report. Ocular Surface, 2017, 15(3): 366–403. doi: 10.1016/j.jtos.2017.03.006
|
| [8] |
ARITA R. Special collection from the lid and meibomian gland working group. Ocular Surface, 2020, 18(2): 191–192. doi: 10.1016/j.jtos.2020.01.002
|
| [9] |
BRON AJ, DE PAIVA CS, CHAUHAN SK, et al. TFOS DEWS II pathophysiology report. Ocular Surface, 2017, 15(3): 438–510. doi: 10.1016/j.jtos.2017.05.011
|
| [10] |
BROWN SH, KUNNEN CM, PAPAS EB, et al. Intersubject and interday variability in human tear and meibum lipidomes: a pilot study. Ocular Surface, 2016, 14(1): 43–48. doi: 10.1016/j.jtos.2015.08.005
|
| [11] |
CRAIG JP, NICHOLS KK, AKPEK EK, et al. TFOS DEWS II definition and classification report. Ocular Surface, 2017, 15(3): 276–283. doi: 10.1016/j.jtos.2017.05.008
|
| [12] |
BUTOVICH IA, SUZUKI T, WOJTOWICZ J, et al. Comprehensive profiling of Asian and Caucasian meibomian gland secretions reveals similar lipidomic signatures regardless of ethnicity. Scientific Reports, 2020, 10(1): 14510. doi: 10.1038/s41598-020-71259-5
|
| [13] |
KIM JH, SHIN YU, SEONG M, et al. Eyelid changes related to meibomian gland dysfunction in early middle-aged patients using topical glaucoma medications. Cornea, 2018, 37(4): 421–425. doi: 10.1097/ICO.0000000000001489
|
| [14] |
SABETI S, KHEIRKHAH A, YIN J, et al. Management of meibomian gland dysfunction: a review. Survey of Ophthalmology, 2020, 65(2): 205–217. doi: 10.1016/j.survophthal.2019.08.007
|
| [15] |
EOM Y, NA KS, HWANG HS, et al. Clinical efficacy of eyelid hygiene in blepharitis and meibomian gland dysfunction after cataract surgery: a randomized controlled pilot trial. Scientific Reports, 2020, 10(1): 11796. doi: 10.1038/s41598-020-67888-5
|
| [16] |
TANABE H, KAIDO M, KAWASHIMA M, et al. Effect of eyelid hygiene detergent on obstructive meibomian gland dysfunction. Journal of Oleo Science, 2019, 68(1): 67–78. doi: 10.5650/jos.ess18161
|
| [17] |
ARYASIT O, UTHAIRAT Y, SINGHA P, et al. Efficacy of baby shampoo and commercial eyelid cleanser in patients with meibomian gland dysfunction: a randomized controlled trial. Medicine (Baltimore), 2020, 99(19): e20155. doi: 10.1097/MD.0000000000020155
|
| [18] |
XIE WJ, JIANG LJ, ZHANG X, et al. Eyelid margin cleaning using deep cleaning device for the treatment of meibomian gland dysfunction-associated dry eye: a preliminary investigation. Journal of Zhejiang University-Science B (Biomedicine & Biotechnology), 2019, 20(8): 679–686. doi: 10.1631/jzus.B1900091
|
| [19] |
AMBAW YA, FUCHS D, RAIDA M, et al. Changes of tear lipid mediators after eyelid warming or thermopulsation treatment for meibomian gland dysfunction. Prostaglandins Other Lipid Mediators, 2020, 151: 106474. doi: 10.1016/j.prostaglandins.2020.106474
|
| [20] |
MURPHY O, O' DWYER V, LLOYD-MCKERNAN A. The efficacy of warm compresses in the treatment of meibomian gland dysfunction and demodex folliculorum blepharitis. Current Eye Research, 2020, 45(5): 563–575. doi: 10.1080/02713683.2019.1686153
|
| [21] |
WANG M, FENG J, WONG J, et al. Randomised trial of the clinical utility of an eyelid massage device for the management of meibomian gland dysfunction. Contact Lens Anterior Eye, 2019, 42(6): 620–624. doi: 10.1016/j.clae.2019.07.008
|
| [22] |
LI B, FU H, LIU T, et al. Comparison of the therapeutic effect of meibomian thermal pulsation LipiFlow® on obstructive and hyposecretory meibomian gland dysfunction patients. International Ophthalmology, 2020, 40(12): 3469–3479. doi: 10.1007/s10792-020-01533-y
|
| [23] |
TAUBER J, OWEN J, BLOOMENSTEIN M, et al. Comparison of the iLUX and the LipiFlow for the treatment of meibomian gland dysfunction and symptoms: a randomized clinical trial. Clinical Ophthalmology, 2020, 14: 405–418. doi: 10.2147/OPTH.S234008
|
| [24] |
KIM HJ, PARK JH. Clinical efficacy of immediate manual meibomian gland expression after thermal pulsation (LipiFlow) for obstructive meibomian gland dysfunction: comparison with thermal pulsation. Cornea, 2020, 39(8): 975–979.
|
| [25] |
BLACKIE CA, COLEMAN CA, NICHOLS KK, et al. A single vectored thermal pulsation treatment for meibomian gland dysfunction increases mean comfortable contact lens wearing time by approximately 4 hours per day. Clinical Ophthalmology, 2018, 12: 169–183. doi: 10.2147/OPTH.S153297
|
| [26] |
HAGEN KB, BEDI R, BLACKIE CA, et al. Comparison of a single-dose vectored thermal pulsation procedure with a 3-month course of daily oral doxycycline for moderate-to-severe meibomian gland dysfunction. Clinical Ophthalmology, 2018, 12: 161–168. doi: 10.2147/OPTH.S150433
|
| [27] |
PANG SP, CHEN YT, TAM KW, et al. Efficacy of vectored thermal pulsation and warm compress treatments in meibomian gland dysfunction: a meta-analysis of randomized controlled trials. Cornea, 2019, 38(6): 690–697. doi: 10.1097/ICO.0000000000001907
|
| [28] |
TASHBAYEV B, YAZDANI M, ARITA R, et al. Intense pulsed light treatment in meibomian gland dysfunction: a concise review. Ocular Surface, 2020, 18(4): 583–594. doi: 10.1016/j.jtos.2020.06.002
|
| [29] |
PIYACOMN Y, KASETSUWAN N, REINPRAYOON U, et al. Efficacy and safety of intense pulsed light in patients with meibomian gland dysfunction - a randomized, double-masked, sham-controlled clinical trial. Cornea, 2020, 39(3): 325–332. doi: 10.1097/ICO.0000000000002204
|
| [30] |
XUE AL, WANG M, ORMONDE SE, et al. Randomised double-masked placebo-controlled trial of the cumulative treatment efficacy profile of intense pulsed light therapy for meibomian gland dysfunction. Ocular Surface, 2020, 18(2): 286–297. doi: 10.1016/j.jtos.2020.01.003
|
| [31] |
YAN X, HONG J, JIN X, et al. The efficacy of intense pulsed light combined with meibomian gland expression for the treatment of dry eye disease due to meibomian gland dysfunction: a multicenter, randomized controlled trial. Eye & Contact Lens: Science & Clinical Practice, 2020. doi: 10.1097/icl.0000000000000711.
|
| [32] |
ARITA R, FUKUOKA S, MORISHIGE N. Therapeutic efficacy of intense pulsed light in patients with refractory meibomian gland dysfunction. Ocular Surface, 2019, 17(1): 104–110. doi: 10.1016/j.jtos.2018.11.004
|
| [33] |
WU Y, LI J, HU M, et al. Comparison of two intense pulsed light patterns for treating patients with meibomian gland dysfunction. International Ophthalmology, 2020, (40): 1695–1705.
|
| [34] |
YIN Y, GONG L. Reversibility of gland dropout and significance of eyelid hygiene treatment in meibomian gland dysfunction. Cornea, 2017, 36(3): 332–337. doi: 10.1097/ICO.0000000000001042
|
| [35] |
WELLING JD, MAUGER TF, SCHOENFIELD LR, et al. Chronic eyelid dermatitis secondary to cocamidopropyl betaine allergy in a patient using baby shampoo eyelid scrubs. JAMA Ophthalmology, 2014, 132(3): 357–359. doi: 10.1001/jamaophthalmol.2013.6254
|
| [36] |
KAIDO M, IBRAHIM OM, KAWASHIMA M, et al. Eyelid cleansing with ointment for obstructive meibomian gland dysfunction. Japanese Journal of Ophthalmology, 2017, 61(1): 124–130. doi: 10.1007/s10384-016-0477-6
|
| [37] |
JONES L, DOWNIE LE, KORB D, et al. TFOS DEWS II management and therapy report. Ocular Surface, 2017, 15(3): 575–628. doi: 10.1016/j.jtos.2017.05.006
|
| [38] |
WANG M, LIU LJ, MCPHERSON RD, et al. Therapeutic profile of a latent heat eyelid warming device with temperature setting variation. Contact Lens Anterior Eye, 2020, 43(2): 173–177. doi: 10.1016/j.clae.2019.09.004
|
| [39] |
NGO W, SRINIVASAN S, JONES L. An eyelid warming device for the management of meibomian gland dysfunction. Journal of Optometry, 2019, 12(2): 120–130. doi: 10.1016/j.optom.2018.07.002
|
| [40] |
WANG DH, LIU XQ, HAO XJ, et al. Effect of the meibomian gland squeezer for treatment of meibomian gland dysfunction. Cornea, 2018, 37(10): 1270–1278. doi: 10.1097/ICO.0000000000001682
|
| [41] |
LEE H, KIM M, PARK SY, et al. Mechanical meibomian gland squeezing combined with eyelid scrubs and warm compresses for the treatment of meibomian gland dysfunction. Clinical Experimental Optometry, 2017, 100(6): 598–602. doi: 10.1111/cxo.12532
|
| [42] |
ZHANG SD, HE JN, NIU TT, et al. Effectiveness of meibomian gland massage combined with topical levofloxacin against ocular surface flora in patients before penetrating ocular surgery. Ocular Surface, 2018, 16(1): 70–76. doi: 10.1016/j.jtos.2017.09.001
|
| [43] |
LIU S, TANG S, DONG H, et al. Intense pulsed light for the treatment of meibomian gland dysfunction: a systematic review and meta-analysis. Experimental and Therapeutic Medicine, 2020, 20(2): 1815–1821. doi: 10.3892/etm.2020.8838
|
| [44] |
ALBIETZ JM, SCHMID KL. Intense pulsed light treatment and meibomian gland expression for moderate to advanced meibomian gland dysfunction. Clinical Experimental Optometry, 2018, 101(1): 23–33. doi: 10.1111/cxo.12541
|
| [45] |
SUWAL A, HAO JL, ZHOU DD, et al. Use of Intense pulsed light to mitigate meibomian gland dysfunction for dry eye disease. International Journal of Medical Sciences, 2020, 17(10): 1385–1392. doi: 10.7150/ijms.44288
|
| [46] |
WLADIS EJ, AAKALU VK, FOSTER JA, et al. Intense pulsed light for meibomian gland disease: a report by the American academy of ophthalmology. Ophthalmology, 2020, 127(9): 1227–1233. doi: 10.1016/j.ophtha.2020.03.009
|
| [47] |
YIN Y, LIU N, GONG L, et al. Changes in the meibomian gland after exposure to intense pulsed light in meibomian gland dysfunction (MGD) patients. Current Eye Research, 2018, 43(3): 308–313.
|
| [48] |
LEE H, HAN YE, PARK SY, et al. Changes in the expression of matrix metalloproteinase-9 after intense pulsed light therapy combined with meibomian gland expression in moderate and severe meibomian gland dysfunction. Contact Lens & Anterior Eye, 2020. doi: 10.1016/j.clae.2020.05.008.
|
| [49] |
GE J, LIU N, WANG X, et al. Evaluation of the efficacy of optimal pulsed technology treatment in patients with cataract and meibomian gland dysfunction in the perioperative period. BMC Ophthalmology, 2020, 20(1): 111. doi: 10.1186/s12886-020-01357-5
|
| [50] |
COTE S, ZHANG AC, AHMADZAI V, et al. Intense pulsed light (IPL) therapy for the treatment of meibomian gland dysfunction. the Cochrane Database of Systematic Reviews, 2020, doi: 10.1002/14651858.CD013559.
|
| [51] |
INCEKALAN TK, HARBIYELI II, YAGMUR M, et al. Effectiveness of intraductal meibomian gland probing in addition to the conventional treatment in patients with obstructive meibomian gland dysfunction. Ocular Immunology and Inflammation, 2019, 27(8): 1345–1351. doi: 10.1080/09273948.2018.1522357
|
| [52] |
KHEIRKHAH A, KOBASHI H, GIRGIS J, et al. A randomized, sham-controlled trial of intraductal meibomian gland probing with or without topical antibiotic/steroid for obstructive meibomian gland dysfunction. Ocular Surface, 2020, 18(4): 852–856. doi: 10.1016/j.jtos.2020.08.008
|
| [53] |
SHEN G, QI Q, MA X. Effect of moisture chamber spectacles on tear functions in dry eye disease. Optometry and Vision Science, 2016, 93(2): 158–164. doi: 10.1097/OPX.0000000000000778
|
| [54] |
MOON CH, KIM JY, KIM MJ, et al. Effect of three-dimensional printed personalized moisture chamber spectacles on the periocular humidity. Journal of Ophthalmology, 2016, 5039181.
|
| [55] |
CHENG J, LI Q, REN LH, et al. Clinical observation of eye acupuncture combined with conventional acupuncture on dry eye syndrome with yin deficiency of liver and kidney. Chinese Acupuncture & Moxibustion, 2019, 39(9): 945–949.
|
| [56] |
WU LH, WANG Y, SHANG SS, et al. Influence of acupuncture treatment on the content of CXCR3 and CXCL10 of dry eye patients caused by MGD. Chinese Journal of Medicine, 2018, 53(11): 1273–1276.
|
| [57] |
HE J, WEN R. Efficacy of external fumigation in treating xerophthalmia caused by meibomian gland dysfunction. Journal of Liaoning University of Traditional Chinese Medicine, 2018, 20(11): 203–205.
|
| [58] |
HANG J, YAO YR, QIAN J, et al. Clinical investigation on meibomian gland dysfunction treated with mingmu decoction steaming and hot compression. China Journal of Chinese Ophthalmology, 2018, 28(4): 229–232.
|
| [59] |
LI R. Analysis the efficacy and action mechanism of thunder-fire moxibustion on dry eye with oculus keratograph. Fujian University of Traditional Chinese Medicine, 2015, 24(8): 1961–1962.
|
| [60] |
KIM BH, KIM MH, KANG SH, et al. Optimizing acupuncture treatment for dry eye syndrome: a systematic review. BMC Complement and Alternative Medicine, 2018, 18(1): 145. doi: 10.1186/s12906-018-2202-0
|
| [61] |
MA XJ, ZHAO YD, ZHANG GX, et al. The rules of acupoint selection of acupuncture for dry eye. Zhongguo Zhen Jiu, 2019, 39(1): 87–90.
|
| [62] |
DHALIWAL DK, ZHOU S, SAMUDRE SS, et al. Acupuncture and dry eye: current perspectives. a double-blinded randomized controlled trial and review of the literature. Clinical Ophthalmology, 2019, 13: 731–740. doi: 10.2147/OPTH.S175321
|
| [63] |
ZHU Y, ZHAO Q, JIA H, et al. Acupuncture for the treatment of dry eye: protocol for systematic review and meta-analysis. Medicine (Baltimore), 2020, 99(32): e21625. doi: 10.1097/MD.0000000000021625
|
| [64] |
ZHU D, GAO C, ZHONG YM. Clinical observation of dry eye syndrome treated with acupuncture. Chinese Acupuncture & Moxibustion, 2019, 39(8): 837–840.
|
| [65] |
WANG X, FAN Y, LAN H, et al. The efficacy and safety of acupuncture or combined with western medicine for dry eye: a protocol for systematic review and meta-analysis. Medicine (Baltimore), 2020, 99(35): e21878. doi: 10.1097/MD.0000000000021878
|
| [66] |
FU H, WANG J, ZHANG F, et al. Effect of acupuncture versus artificial tears for dry eye disease: a protocol for systematic review and meta-analysis. Medicine (Baltimore), 2020, 99(30): e21301. doi: 10.1097/MD.0000000000021301
|
| [67] |
LIU CY, QIN S, GAO WP, et al. Effect of acupuncture on expression of transfer growth factor-β1 in lacrimal gland of rabbits with dry eye. Acupuncture Research, 2020, 45(9): 726–730.
|
| [68] |
WEI QB, DING N, WANG JJ, et al. Acupoint selection for the treatment of dry eye: a systematic review and meta-analysis of randomized controlled trials. Experimental and Therapeutic Medicine, 2020, 19(4): 2851–2860.
|
| [69] |
ZHANG D, ZHAO Y, YANG YT, et al. A mechanism study of electroacupuncture for dry eye syndrome by targeting conjunctival cytokine expressions. Current Eye Research, 2020, 45(4): 419–427. doi: 10.1080/02713683.2019.1666997
|
| [70] |
KEWEI WU, JIANG Y, MAO D, et al. Clinical study on Qiju Dihuang Tang combined with fumigation by ultrasonic atomization for dry eye after phacoemulsification. Journal of New Chinese Medicine, 2019, 546(11): 201–204.
|
| [71] |
HONG-JIE MA, ZHENG YL. New progress in the research of dry eye treatment with traditional Chinese medicine. China Journal of Traditional Chinese Medicine & Pharmacy, 2018, 33(4): 1469–1473.
|
| [72] |
XU-CHUN LIU, CHEN-CHONG DA, LU-XIN AN. Effect of TCM fumigation combined with meibomian gland massage in the treatment of dry eye. Chinese Journal of Traditional Medical Science and Technology, 2019, 26(1): 146–147.
|
| [73] |
LV XP, DU C, ZHANG YJ, et al. Treatment of meibomian gland dysfunction xerophthalmia with traditional Chinese medicine mask fumigation combined with tarsal gland massage. Zhejiang Journal of Integrated Traditional Chinese and Western Medicine, 2018, 28(2): 119–121.
|
| [74] |
HOU DS. Clinical observation of pluralistic treatment of meibomian gland dysfunction xerophthalmia. Journal of Community Medicine, 2018, 16(17): 1352–1356.
|
| [75] |
CHEN YY, HUANG C, FENG YH, et al. Fumigation treatment of Four Yellow Qing Ling Water with artificial tears for dry eye. International Eye Science, 2018, 18(4): 762–764.
|
| [76] |
ZI Y, JI M, DENG Y, et al. The effectiveness and safety of moxibustion for dry eye: protocol for a systematic review. Medicine (Baltimore), 2019, 98(15): e15178. doi: 10.1097/MD.0000000000015178
|
| [77] |
FU W, ZHANG G, LIU Z, et al. Walnut-shell moxibustion for dry eye symptoms: a randomized controlled trial. Chinese Acupuncture & Moxibustion, 2018, 38(11): 1177–1182.
|
| [78] |
ZHANG Y, YUE LJ, TANG M, et al. Clinical effect of traditional Chinese medicine in treating dry eye disease with eye-fumigation combined with thunder-fire moxibustion. World Chinese Medicine, 2018, 13(2): 348–351, 355.
|
| [79] |
ZI Y, JI M, DENG Y, et al. The effectiveness and safety of moxibustion for dry eye: protocol for a systematic review. Medicine (Abingdon), 2019, 98(15): e15178.
|
| [80] |
QIAN LJ, ZHU SN, ZHANG YT. Clinical observation of thunder fire moxibustion combined with tobramycin dexamethasone eye drops for the treatment of meibomian gland dysfunction. Journal of New Chinese Medicine, 2018, 50(1): 77–80.
|
| [81] |
WANG CL, CONG SP. Treatment of 90 cases of menopausal xerophthalmia with traditional Chinese medicine combined with acupoint massage. China's Naturopathy, 2013, 21(7): 48–48.
|
| [82] |
LIU B, CHEN YS. Clinical observation on treatment of dry eye by ultrasonic cooling fog and stick moxibustion. Lishizhen Medicine and Materia Medica Research, 2013, 24(8): 1961–1962.
|
| [1] | FENG Gege, ZHANG Yue, WU Huangan, ZHU Lu, XU Hongxiao, MA Zhe, HUANG Yan. Modulation of colonic DNA methyltransferase by mild moxibustion and electroacupuncture in ulcerative colitis TET2 knockout mice[J]. Digital Chinese Medicine, 2025, 8(1): 100-110. DOI: 10.1016/j.dcmed.2025.03.009 |
| [2] | S. Priyadharshini, A. Mooventhan, Venkatalakshmi Saravanan, N. Mangaiarkarasi. Effects of needling at Sanyinjiao (SP6) acupuncture point on blood glucose levels and cardiovascular functions in patients with type 2 diabetes mellitus: a randomized placebo-controlled study[J]. Digital Chinese Medicine, 2024, 7(3): 224-230. DOI: 10.1016/j.dcmed.2024.12.002 |
| [3] | GONG Changzhen. A Rumsfeld Matrix test for acupuncture clinical trials[J]. Digital Chinese Medicine, 2024, 7(3): 209-223. DOI: 10.1016/j.dcmed.2024.12.001 |
| [4] | WONG Tsz Ho, WEI Junyi, CHEN Haiyong, NG Bacon Fung Leung. A novel deep learning based cloud service system for automated acupuncture needle counting: a strategy to improve acupuncture safety[J]. Digital Chinese Medicine, 2024, 7(1): 40-46. DOI: 10.1016/j.dcmed.2024.04.005 |
| [5] | ZOU Menglong, HU Zhuoyu, LONG Dan, SUN Haoxian, ZHU Ying. Evidence and acupoint combinations in acupuncture for functional dyspepsia: an overview of systematic review and data mining study[J]. Digital Chinese Medicine, 2023, 6(4): 369-380. DOI: 10.1016/j.dcmed.2024.01.001 |
| [6] | SUN Meiling, ZHAO Fanghua, GAO Man, ZHEN Siyuan, CHEN Yueling, Ramon Maria Calduch, LI Haiyan. Hotspots and comparative analysis of international acupuncture research over the past decade via Web of Science[J]. Digital Chinese Medicine, 2023, 6(1): 28-40. DOI: 10.1016/j.dcmed.2023.02.002 |
| [7] | GUO Yi, LI Zhenji, LIU Baoyan, SANG Binsheng, FU Qiang, ZHAO Xue, CHEN Bo, CHEN Zelin, YANG Huayuan, HE Liyun, YANG Yi, LV Zhongqian, ZHAO Tianyi, LI Dan, FU Hua, YUAN Xinru. Establishment of basic principles and methods of acupuncture standardization in traditional Chinese medicine[J]. Digital Chinese Medicine, 2023, 6(1): 3-8. DOI: 10.1016/j.dcmed.2023.04.001 |
| [8] | YUAN Hang, YU Xiaohua, LI Xiang, QIN Sijun, LIANG Guixiang, BAI Tianyu, WEI Benzheng. Research on resting spontaneous brain activity and functional connectivity of acupuncture at uterine acupoints[J]. Digital Chinese Medicine, 2022, 5(1): 59-67. DOI: 10.1016/j.dcmed.2022.03.006 |
| [9] | CHEN Mei, LI Jie, PENG Jun, HUANG Yu, OUYANG Weijie, LIU Xiaoqing, SHEN Zhibin, LI Changdong, WANG Yi, PENG Qinghua. Linarin ameliorates innate inflammatory response in an experimental dry eye model via modulation of the NLRP3 inflammasome[J]. Digital Chinese Medicine, 2021, 4(1): 42-53. DOI: 10.1016/j.dcmed.2021.03.006 |
| [10] | WANG Xue-Song, WANG Yue-Shen, LI Jia-Jia, YU Chao-Chao, WU Miao, KONG Li-Hong. Acupuncture and Related Therapies for Hyperlipidemia: A Network Meta-Analysis[J]. Digital Chinese Medicine, 2020, 3(4): 309-326. DOI: 10.1016/j.dcmed.2020.12.002 |
| 1. | Huang Y., Li J., Li D.-D. et al. Meta-analysis of therapeutic effect of intense pulsed light combined with meibomian gland expression on meibomian gland dysfunction related dry eye. International Eye Science, 2023, 23: 616-623. DOI:10.3980/j.issn.1672-5123.2023.4.17 |
| 2. | Li Z., Wang H., Liang M. et al. Hypochlorous Acid Can Be the Novel Option for the Meibomian Gland Dysfunction Dry Eye through Ultrasonic Atomization. Disease Markers, 2022, 2022 DOI:10.1155/2022/8631038 |
| 3. | Mei C., Jie L., Jun P. et al. Linarin ameliorates innate inflammatory response in an experimental dry eye model via modulation of the NLRP3 inflammasome. Digital Chinese Medicine, 2021, 4: 42-53. DOI:10.1016/j.dcmed.2021.03.006 |
| Therapy | Medical devices | Treatment site | Therapeutic mechanism | Therapeutic effects |
| Eyelid hygiene | Wipes, pumps, gels, solutions, sprays and swabs containing anti-inflammatory, antimicrobial, anti-parasitic and antifungal ingredients | Eyelid margin | Cleanse the eyelid margin and lashes | ③④⑧[15] ⑦⑧[16] ①⑥[17] ①④⑧⑨[18] |
| Eyelid warming and massage | Artificial eyelid warming and massage devices | Both upper and lower external/inner eyelids | Artificial heating and evacuation of the gland contents | ④⑧⑪[19] ②④⑧[20] ②⑤⑪[21] |
| LipiFlow® System | Both upper and lower inner eyelids | Automated heating (42.5 °C) on both inner eyelid surfaces while pulsating pressure to evacuate the gland contents | ①⑥⑫[22] ①⑥⑦[23] ①②⑫[24] | |
| LipiFlow® Vectored Thermal Pulsation (VTP) System | Both upper and lower inner eyelids | Automated heat transfer and simultaneous evacuation of the gland contents while heating the glands to therapeutic levels (≥ 40 °C) | ①④⑥[25] ①④⑩[26] ①④⑧[27] | |
| IPL/OPT | IPL: IPL devices OPT: IPL devices (an optimal model for IPL) | The skin near the eyelids, four overlapping periocular zones under each eye, with the fifth pulse applied temporally adjacent to the lateral canthus | Selective thermal delivery to the meibomian glands and liquefication of the inspissated meibum | ④⑥⑧[28, 29] ⑤⑫[30] ①④[31] ②④⑧[32, 33] |
| ① Improved tear break-up time (TBUT); ② improved corneal or conjunctival fluorescein staining score; ③ improved lid margin lissamine green staining score; ④ improved meibum status or secretion; ⑤ improved eyelid margin and signs; ⑥ reduced ocular surface disease index (OSDI) score; ⑦improved meibomian gland atrophy; ⑧improvements in subjective symptoms; ⑨ improvement in meibomian orifice obstruction; ⑩ improved standard patient evaluation for eye dryness (SPEED) score; ⑪ improved visual analogue scale (VAS) score; ⑫ improved lipid layer thickness. | ||||
| Therapy | Medical devices | Treatment site | Therapeutic mechanism | Therapeutic effects |
| Acupuncture | Needles for acupuncture | Jing Ming (BL1), Cuan Zhu (BL2), Yang Bai (GB14), Si Zhu Kong (TE23), Tai Yang (EX-HN5), Si Bai (ST2), He Gu (LI4), Tai Chong (LR3), Guang Ming (GB37), San Yin Jiao (SP6), Feng Chi (GB20), etc. | Promote meridian circulation, regulate Qi and blood | ①②④⑤[55] ①③[56] |
| Eye fumigation | Eye fumigation devices | Periorbital area and the ocular surface | Spread the external evil, nourish Yin and glory, dredge the meridians and collaterals, and unobstructed Qi and blood | ①③⑥[57] ①③[58] |
| Moxibustion | Moxa-moxibustion, thunder-fire moxibustion, walnut moxibustion, etc. | Periorbital area | dredging meridian, harmonizing Qi and blood, activating blood circulation and removing blood stasis, eliminating inflammation and analgesia | ①②③④[58] ①③[59] |
| ① Improved tear break-up time (TBUT); ② improved corneal or conjunctival fluorescein staining score; ③ increased tear production; ④ improved subjective symptoms; ⑤ improved eyelid margin and signs; ⑥ improved lipid layer thickness. | ||||