| Citation: | Citation: XIE MX, CAI ZY, LI JY, et al. Metabolic characteristics of Qi-Yin deficiency and heat stagnation in liver meridian patterns of dry eye based on tear metabolomics. Digital Chinese Medicine, 2024, 7(3): 274-283. DOI: 10.1016/j.dcmed.2024.12.007 |
To explore the metabolic differences between dry eye patients with Qi-Yin deficiency and heat stagnation in liver meridian patterns, and clarify their metabolic characteristics.
Patients with dry eye who were treated in the Ophthalmology Ward and Outpatient Department of the First Hospital of Hunan University of Chinese Medicine from October 1, 2020, to October 30, 2021 were enrolled as the research participants in the study. They were assigned to two groups based on traditional Chinese medicine (TCM) syndrome types: heat stagnation in liver meridian pattern group and Qi-Yin deficiency pattern group. Healthy volunteers who underwent health check-ups in the Health Management Department were included as healthy group following the random number table method. The tears of the patients and the healthy volunteer participants were tested by high-performance liquid chromatography-mass spectrometry (LC-MS). The differential metabolites were screened out by multivariate statistical analysis, and Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway enrichment was performed on the differential metabolites. Finally, the association analysis of differential proteins and metabolites was conducted to verify and supplement the metabolites.
A total of 32 dry eye patients were enrolled, including 16 cases with heat stagnation in liver meridian pattern and 16 cases with Qi-Yin deficiency pattern. Fourteen healthy volunteers were included as healthy group. There were no significant differences in baseline characteristics among the three groups (P > 0.05). A total of 412 biomarkers were determined in Qi-Yin deficiency pattern group, mainly including lipids, lipid-like molecules, organic acids and their derivatives, organic heterocyclic compounds, and nucleosides and their analogues. For heat stagnation in liver meridian pattern group, 112 metabolites were determined, mainly including organic acids and their derivatives, lipids, and lipid-like molecules. The KEGG enrichment results of pathways and the relative content analysis of differential markers demonstrate that purine metabolism and caffeine metabolism pathways are common metabolic characteristics of all dry eyes. Among them, deoxyinosine monophosphate (dIMP) and 2-(formamido)-N1-(5-phospha-D-ribosyl) acetamidine can serve as their biomarkers. The main characteristics of Qi-Yin deficiency syndrome pattern were the significant enhancement of metabolic pathways such as lysine degradation, ovarian steroidogenesis, cholesterol metabolism, pyrimidine metabolism, and bile secretion (P < 0.05). Dry eye associated with the heat stagnation in liver meridian pattern is mainly characterized by inhibition of the valine, leucine, and isoleucine biosynthesis pathways (P < 0.05).
Metabolomics can be used as an effective basis for TCM syndrome classification. Different patterns of dry eye syndrome exhibit typical characteristics in the types and concentrations of metabolites, which correspond to the syndrome classification in TCM. This study initially confirms the rationality of TCM syndrome classification and provides significant reference for the mechanism of dry eye and drug development.
Dry eye is a multifactorial disease characterized by decreased stability of the tear film and accompanied by ocular discomfort, with complex etiology and pathophysiological mechanisms [1]. The incidence of dry eye in China has reached 21% to 30%, and the demand for its treatment is also increasing year by year [2]. Dry eye is associated with various systemic and metabolic conditions and functional disorders, including vitamin A deficiency, inadequate omega-3 and omega-6 fatty acid intake, ovarian dysfunction, menopause, diabetes, sarcoidosis, and the use of systemic drugs such as antidepressants, antihistamines, beta-blockers, and antidiuretics [3]. Although dry eye is closely related to many diseases, little is known about its molecular biological basis.
Traditional Chinese medicine (TCM) classifies dry eye into categories such as “white xerotic syndrome” “dryness and blurred vision syndrome” and “impending desiccation of spirit water”. Meanwhile, modern TCM diagnostic methods divide dry eye into various syndromes, including insufficiency of lung Yin, heat stagnation in liver meridian, lingering evil heat, and Qi-Yin deficiency [4]. Among these, the excess syndrome is mainly characterized by heat stagnation in liver meridian, while the deficiency syndrome is mainly characterized by the Qi-Yin deficiency, demonstrating an increasing trend [5]. Different syndromes require corresponding drug treatments, and their prescriptions are completely varied. Understanding the molecular biological basis of different syndromes of dry eye using modern methods is of great importance for developing diagnostic criteria and detection methods for various syndromes of dry eye.
Advanced high-throughput omics methods (genomics, transcriptomics, proteomics, and metabolomics) have developed greatly, which strengthened our understanding of complex diseases markedly. For example, VEHOF et al. [6] used gas chromatography and liquid chromatography coupled with mass spectrometry to analyze serum samples from 2 819 individuals. Among the 222 metabolites detected, a significant correlation was found between all five androgens and dry eye, leading authors to suggest 1-palmitoyl-sn-glycero-3-phosphocholine as a potential biomarker. Furthermore, the use of nano-liquid chromatography and quadrupole time-of-flight tandem mass spectrometry (nano-LC-Q-TOF-MS/MS) and ultra-performance LC-Q-TOF-MS/MS (UPLC-Q-TOF-MS/MS) techniques in proteomics and metabolomics analyses of tear fluid from patients with dry eye identified 34 metabolites as markers. These were notably related to proteins involved in immune and inflammatory processes. Concurrently, pathways including the complement and coagulation cascade, glycolysis/gluconeogenesis, and amino acid metabolism were associated with dry eye [7]. These findings not only provide diagnostic and therapeutic references for potential biomarkers of dry eye but also promote our understanding of its physiological and pathological mechanisms. However, there is a significant gap in research exploring the molecular biological underpinnings of dry eye across various TCM syndromes.
Therefore, this study aimed to investigate the metabolic profiles in tears of dry eye patients with either heat stagnation in liver meridian pattern or Qi-Yin deficiency pattern using non-targeted metabolomics (UPLC-Q-TOF-MS/MS) and protein-metabolite integrated analysis.
Patients with dry eye who were treated in the Ophthalmology Ward and Outpatient Department of the First Hospital of Hunan University of Chinese Medicine from October 1, 2020, to October 30, 2021 were enrolled as the research participants in the study. They were assigned to two groups based on TCM syndrome types: heat stagnation in liver meridian pattern group and the Qi-Yin deficiency pattern group. Healthy volunteers who underwent health check-ups in the Health Management Department were included as healthy group using a random number table method. All patients voluntarily participated in the study and signed the written informed consent. The study was conducted in accordance with the Declaration of Helsinki and was approved by the Medical Ethics Committee of the First Hospital of Hunan University of Chinese Medicine (HN-LL-SWST-2020-10), and registered with the Chinese Clinical Trial Registry (ChiCTR2100046380). Data sharing is available for this study.
In line with the Chinese Consensus on the Treatment of Dry Eye (2020) [2], the diagnosis of dry eye is based on the following criteria: (i) the main complaint includes one or more symptoms such as eye fatigue, blurred vision, foreign body sensation, or pain; (ii) tear film break-up time (BUT) is ≤ 10 s or Schirmer I test (SIT) ≤ 2 mm/min; (iii) corneal staining assessed with sodium fluorescein shows more than 5 staining points. A diagnosis can be established if any one of these criteria is met.
Based on Traditional Chinese Medicine and Ophthalmology [8], the diagnostic criteria of dry eye are as follows.
(i) Heat stagnation in liver meridian pattern of dry eye. (a) Main symptoms: dryness and burning pain in the eyeballs, slight redness of the white part of the eye, nebulae on the black part of the eye, or intolerance to prolonged viewing. (b) Secondary symptoms: bitter taste in the mouth, dry throat, irritability/easy anger, insomnia/frequent dreams, dry stool, yellow urine; tongue red with thin yellow or thick yellow fur, thready or deep and thready pulse.
(ii) Qi-Yin deficiency pattern of dry eye. (a) Main symptoms: dryness and discomfort in the eyes, lack of luster in the eyes, frequent blinking, photophobia, slight redness of the white part of the eye, intolerance to prolonged viewing, worsening symptoms after prolonged viewing, potential blurring of vision, potential nebulae or filaments on the black part of the eye, difficulty in healing. (b) Secondary symptoms: dry mouth with little saliva, fatigue, dizziness, tinnitus, weakness in the lower back and knees; tongue light red with thin fur, pulse thin or deep and thin.
(i) People who met the above diagnostic criteria; (ii) age between 18 and 75 years; (iii) signed informed consent.
(i) Patients with other ocular diseases, such as blepharitis and congenital anhidrosis; (ii) patients with a history of primary liver, kidney, heart, or lung diseases; (iii) patients with immune system abnormalities, such as Sjögren's syndrome and systemic lupus erythematosus; (iv) patients who have undergone eye surgery in the past three months; (v) patients who have used drugs affecting tear secretion within the past one month.
(i) Healthy individuals without ocular surface symptoms, visual function symptoms, or ciliary muscle irritation symptoms; (ii) normal anterior segment tissue on slit lamp examination; (iii) BUT > 10 s; (iv) SIT > 2 mm/min; (v) signed informed consent.
(i) Symptoms such as dryness, foreign body sensation, fatigue, itching, and swelling in the ocular surface; (ii) symptoms of ciliary muscle irritation like photophobia, pain, tearing, redness of the eye, and stinging sensation; (iii) symptoms of visual function abnormalities such as blurred vision; (iv) a history of meibomian gland dysfunction and dry eye; (v) meeting any of the exclusion criteria for dry eye.
Methanol, formic acid, and acetonitrile were purchased from Thermo Fisher Scientific, USA. L-2-chlorophenylalanine was purchased from Shanghai Hengchuang Biotechnology Co., Ltd., China. All chemicals and solvents were of analytical or chromatographic grade. Instruments were purchased from the following manufacturers: ultrasonic cleaner (F-060SD, Shenzhen Fuyang Technology Group Co., Ltd.); vortex oscillator (TYXH-I, Shanghai Hanuo Instrument Co., Ltd.); desktop high-speed freezing centrifuge (TGL-16MS, Shanghai Luxiangyi Centrifuge Instrument Co., Ltd.); high-resolution mass spectrometer (QE, Thermo Fisher Scientific); high-performance liquid chromatograph (ACQUITY UPLC I-Class PLUS, Waters); chromatographic column (ACQUITY UPLC HSS T3,100 mm × 2.1 mm, 1.8 μm; Waters).
Before collecting specimens, patients were asked to rest in the examination restroom for 15 min and avoid rubbing their eyes. The capillary glass tube method was employed, with a precise quantitative glass capillary gently contacting the lower eyelid margin tear triangle area [9]. The tear fluid entered the tube through capillary action, and then the collected tear fluid was transferred to a 0.2 mL Eppendorf (EP) tube. The amount of tear fluid collected was approximately 50 μL, and the tear fluid samples were stored in a – 80 °C freezer.
The samples designated for testing, previously stored at – 80 °C were thawed at 4 °C. Each sample was transferred 20 μL, and 10 μL of internal standard (L-2-chlorophenylalanine, 0.06 mg/mL; methanol as solvent) was added, vortexed (2 600 rpm, 4 °C, 10 s); 150 μL of methanol-water (V : V = 4 : 1) was added, vortexed for 1 min; ultrasonic extraction in an ice water bath for 10 min, left at – 20 °C for 30 min. After centrifugation (
The mobile phase consisted of A-water (containing 0.1% formic acid) and B-acetonitrile (containing 0.1% formic acid). The initial gradient of the chromatographic conditions was set at 95% A, held for 2 min, then decreased to 70% A at 4 min, to 50% A at 8 min, to 20% A at 10 min, and to 0% A at 14 min, where it was held for an additional 1 min. The column temperature was maintained at 45 °C, with a flow rate of 0.35 mL/min and an injection volume of 5 μL. The mass spectrometer ion source was electrospray lonization (ESI), set at a temperature of 200 °C, and the sample mass spectrometry signal acquisition was performed in both positive (ESI+) and negative (ESI−) ion scanning modes. The mass spectrometry acquisition range was set from 100 to 1 200 m/z, with a full scan resolution of 70 000 and a secondary mass spectrometry resolution of 17 500. The spray voltage for positive ions was
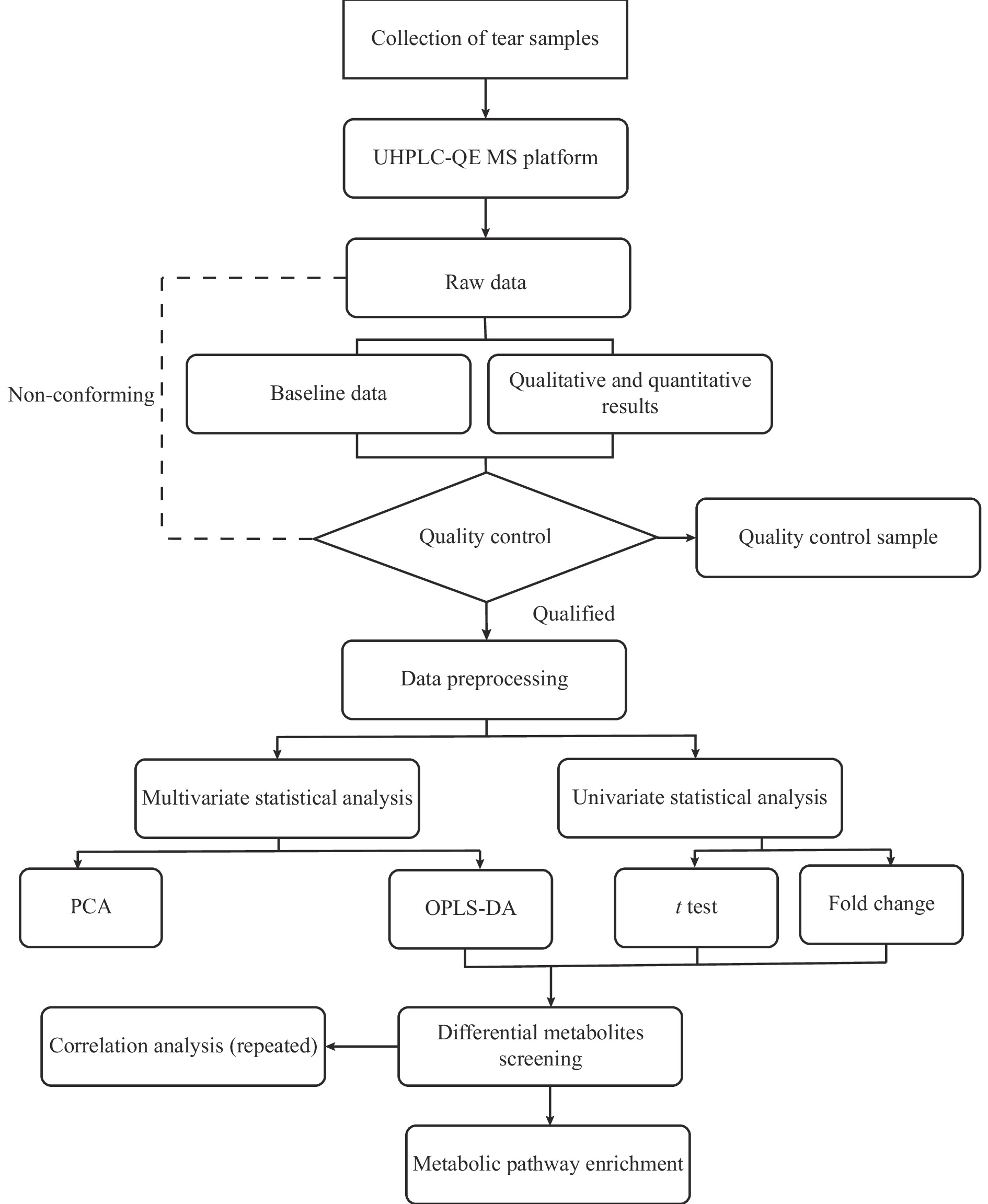
In this study, tear samples were collected from participants and analyzed using the ultra performance liquid chromatography-quadrupole/electrostatic field orbitrap mass spectrometry (UHPLC-QE MS) platform for ESI+ and ESI− modes to obtain data. The raw data were processed using the metabolomics processing software Progenesis QI V2.3 for baseline filtering, peak identification, integration, retention time correction, peak alignment, and normalization. The identification of compounds is based on accurate mass numbers, secondary fragments, and isotopic distributions. Qualitative analysis is performed using databases such as the Human Metabolome Database (HMDB, http://www.hmdb.ca/), LipidMaps, METLIN, and in-house libraries. Compounds are then scored based on the qualitative results, with a screening criterion of 36 points (out of a maximum of 60 points). Compounds with scores below 36 are considered inaccurately identified and are removed. For the extracted data, ion peaks with intra-group missing values (0-values) > 50% are deleted, and 0-values are replaced with half of the minimum value. Finally, the positive and negative ion data are combined into a single data matrix table, which contains all the information extracted from the raw data that can be used for analysis. Multivariate statistical analysis first employs unsupervised principal component analysis (PCA) to observe the overall distribution between samples and the stability of the entire analysis process, followed by supervised orthogonal partial least squares discriminant analysis (OPLS-DA) to distinguish the overall differences in metabolic profiles between groups, identifying differentially expressed metabolites. A combination of multi-dimensional and single-dimensional analysis methods is used to screen for differentially expressed metabolites between groups. Metabolites are extracted based on fold change (FC) > 1.2 and P < 0.05 criteria, and visualized using volcano plots and heat maps. Metabolites with significant differences are then selected using a variable importance in projection (VIP) threshold > 1 and P < 0.05, and pathway analysis is performed. This study utilizes the MetaboAnalyst 5.0 online data analysis website (https://www.metaboanalyst.ca/) for analysis, which is a tool for pathway enrichment exploration and visualization of changes in metabolites. Selected marker metabolites undergo KEGG pathway enrichment analysis, and pathways are selected based on enrichment factors and P-values, with a criterion of P < 0.05. The research flow chart is shown in Figure 1.
Statistical analysis was performed using SPSS 26.0. Measurement data that followed a normal distribution were presented as mean ± standard deviation (SD). The t test was used for testing methods with a significance level of α = 0.05. P < 0.05 was considered statistically significant.
In this experiment, a total of 32 dry eye patients were enrolled, including 16 cases with heat stagnation in liver meridian pattern group and 16 cases with Qi-Yin deficiency pattern group. Fourteen healthy volunteers were included as healthy group. No statistically significant differences were observed in baseline data (age, gender, lifestyle, medication method, and disease course) among the three groups of participants (P > 0.05).
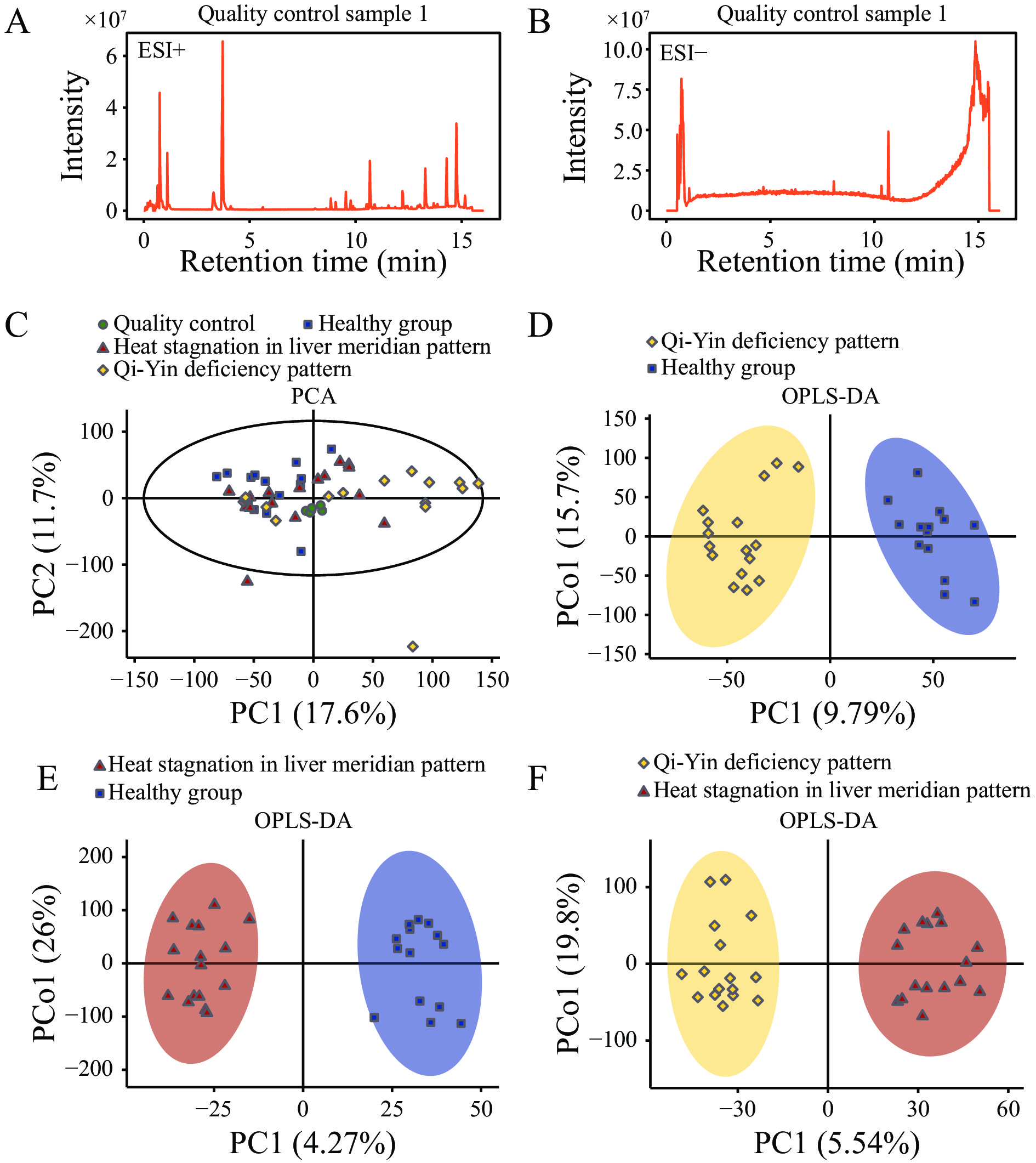
The metabolic data of the three groups were obtained via the LC-MS analysis, covering all metabolites under both ESI+ ion mode and ESI− ion mode. A total of 12 238 positive ion characteristic peaks (3 556 metabolites) and 5 834 negative ion characteristic peaks (1 122 metabolites) were identified, mainly including lipids, lipid molecules, organic acids, and their derivatives (Figure 2A and 2B). A principal component analysis showed that the Qi-Yin deficiency and the heat stagnation in liver meridian patterns of dry eye were clearly separated from healthy group in the metabolic profile, located in the top left and bottom right corners, respectively (Figure 2C). The OPLS-DA model further confirmed this difference, with the R2Y value of 0.935 and Q2 value of 0.644 for the Qi-Yin deficiency type of dry eye versus the control group (Figure 2D), and the R2Y value of 0.96 and Q2 value of 0.47 for the heat stagnation in liver meridian type of dry eye versus the control group (Figure 2E), indicating the reliability of the two established OPLS-DA models. Furthermore, the OPLS-DA model between the Qi-Yin deficiency and the heat stagnation in liver meridian patterns of dry eye patients also met the requirements and could be used for further screening of differential metabolites and analysis of metabolic characteristics (Figure 2F).
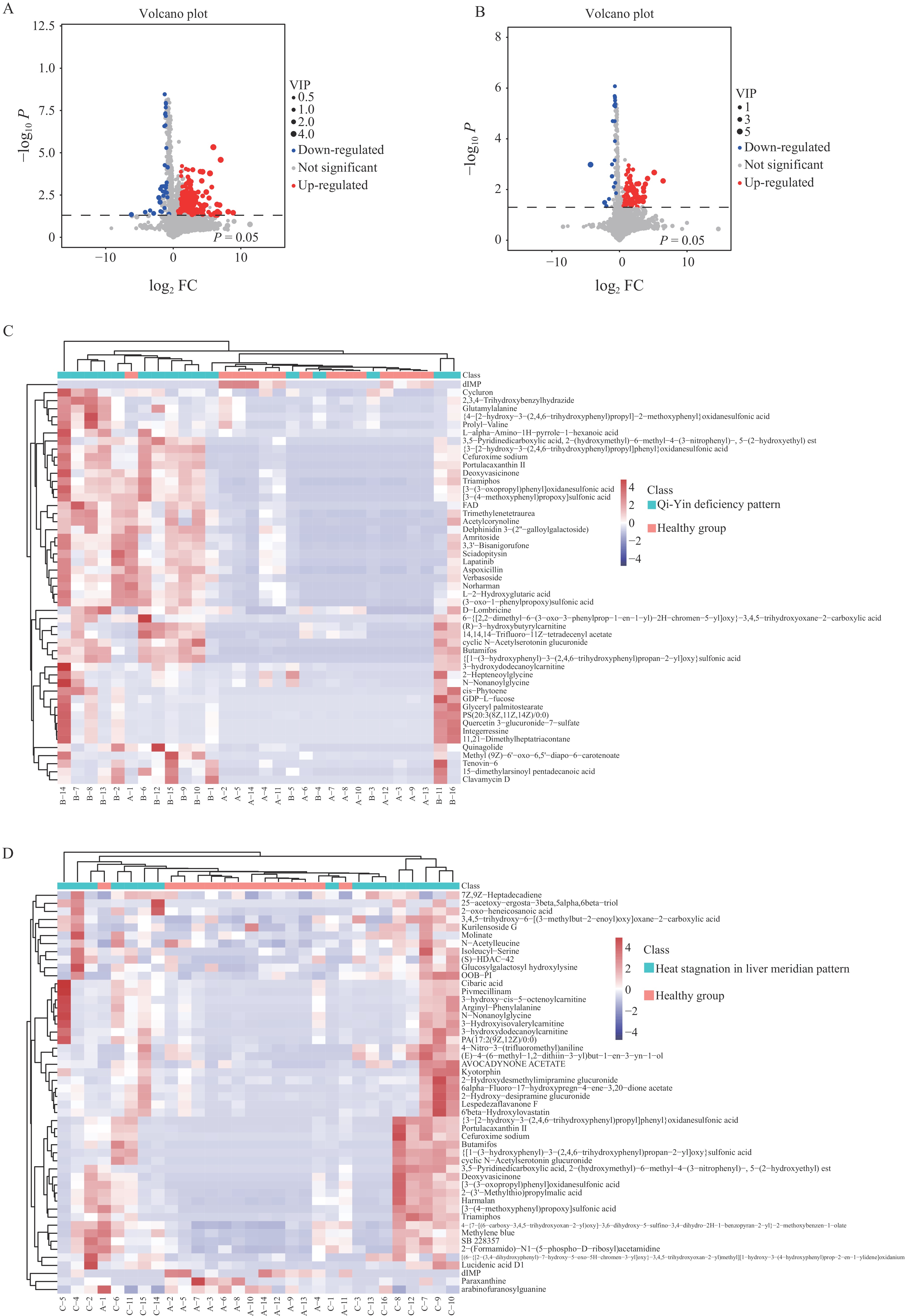
This study extracted metabolites with significant differences and visualized them using volcano plots (Figure 3A and 3B). Overall, 412 markers were identified and confirmed in the comparison between the Qi-Yin deficiency pattern and healthy group, including 294 and 118 metabolites from ESI+ and ESI− models, respectively (Figure 3C). According to the chemical classification method in the HMDB, they were divided into 10 subcategories, among which the significantly different metabolites mostly included lipids, lipid-like molecules, organic acids and their derivatives, organic heterocyclic compounds, nucleosides, nucleotides, and analogs.
Similarly, the markers, based on the above criteria, obtained from the comparison model between the heat stagnation in liver meridian pattern and healthy group were identified and confirmed. The comparison between the heat stagnation in liver meridian pattern and healthy group confirmed 112 metabolites, including 89 and 23 metabolites from ESI+ and ESI− models, respectively (Figure 3D). They were divided into 11 subcategories following the chemical classification method in the HMDB, mainly including organic acids and their derivatives, lipids, and lipid-like molecules.
To further demonstrate the common metabolic characteristics of patients with Qi-Yin deficiency and heat stagnation in liver meridian patterns of dry eye, we extracted and analyzed the common differential metabolites between these two syndrome patterns of dry eye and healthy group. The results showed 32 common differential metabolites in both syndrome patterns of dry eye patients, which were mainly concentrated in the categories of lipids, lipid-like molecules, organic acids, and derivatives of organic acids. Further analysis of these common differential metabolites indicated that their expression trends were consistent in both patterns of dry eye, suggesting that they may play an important role in its pathological mechanism.
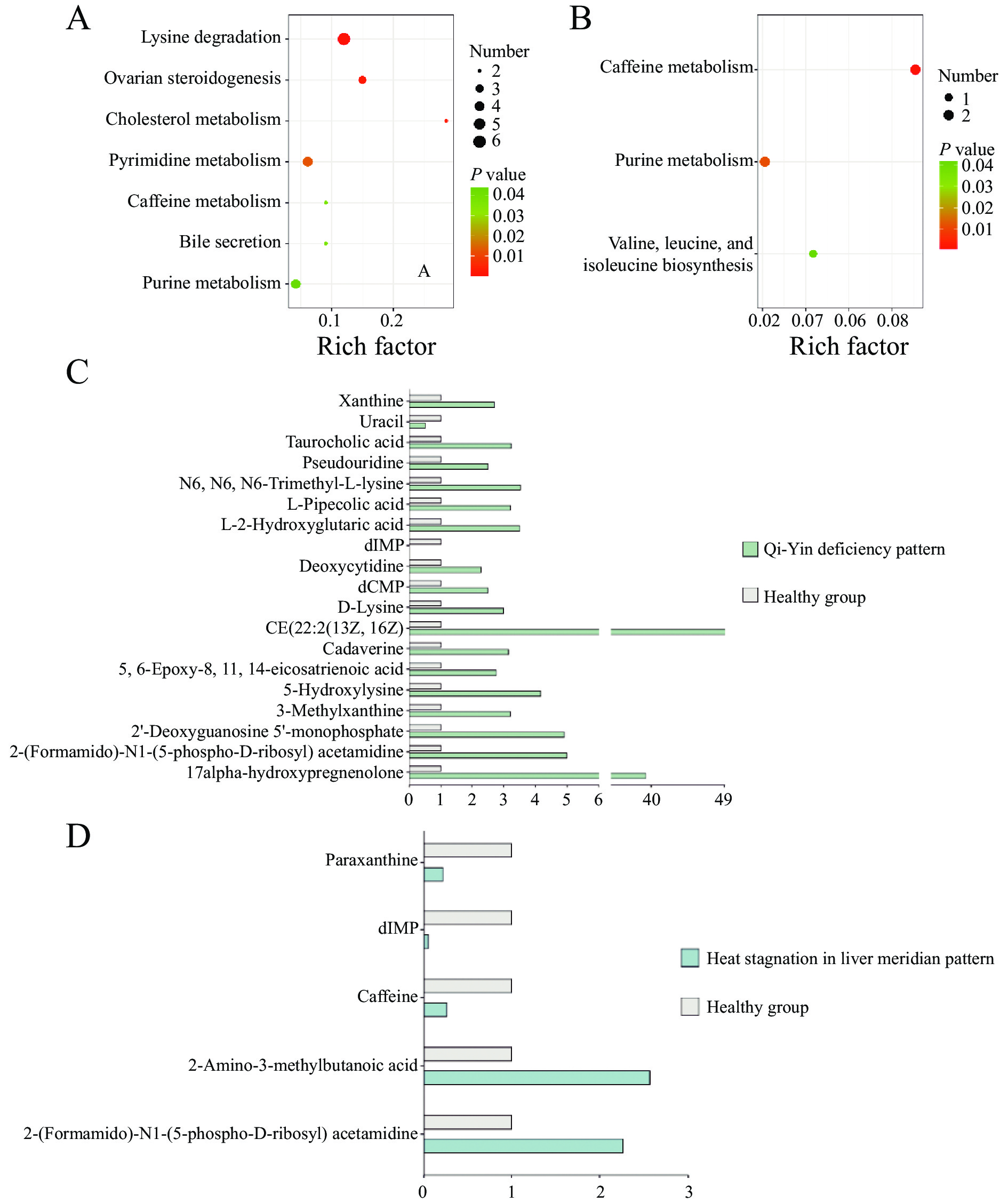
The interrelationships among significantly differential metabolites were further studied, and KEGG pathway enrichment analysis was performed on the selected marker metabolites. Compared with healthy group, the Qi-Yin deficiency pattern group has enriched seven metabolic pathways: lysine degradation, ovarian steroidogenesis, cholesterol metabolism, pyrimidine metabolism, bile secretion, purine metabolism, and caffeine metabolism pathways (Figure 4A). Compared with healthy group, the heat stagnation in liver meridian pattern group has enriched three metabolic pathways: caffeine metabolism, purine metabolism, and valine, leucine, and isoleucine biosynthesis pathways (Figure 4B). The results suggest that purine metabolism and caffeine metabolism pathways may be common pathways in the tear fluid of dry eye; however, the Qi-Yin deficiency pattern and the heat stagnation in liver meridian pattern of dry eye have distinct metabolic characteristics. For example, the typical feature of the heat stagnation in liver meridian pattern of dry eye denotes the difference in valine, leucine, and isoleucine biosynthesis pathways, while the Qi-Yin deficiency pattern of dry eye has a greater variety of different metabolites in the tear fluid.
To further confirm the common metabolic characteristics of dry eye and the metabolic characteristics of the Qi-Yin deficiency and the heat stagnation in liver meridian patterns, this study plotted the relative content graphs of the main differential metabolites in the above-mentioned enriched metabolic pathways. The dIMP and 2-(formamido)-N1-(5-phospho-D-ribosyl) acetamidine, which belong to purine metabolism, showed a consistent trend of change in both patterns, with a significant decrease in deoxyinosine (dIMP) (P < 0.05) and a significant increase in 2-(formamido)-N1-(5-phospho-D-ribosyl) acetamidine (P < 0.05) in dry eye (Figure 4C). For the heat stagnation in liver meridian pattern of dry eye, the typical characteristics contained a significant decrease in caffeine and paraxanthine, which belongs to caffeine metabolism (P < 0.05, Figure 4D), indicating that the inhibition of the caffeine metabolism pathway is one of its typical characteristics. While, the increase in 2-amino-3-methylbutanoic acid, which is a part of the valine, leucine, and isoleucine biosynthesis pathway, indicated that the valine, leucine, and isoleucine biosynthesis pathway may be enhanced in the heat stagnation in liver meridian pattern of dry eye. In the Qi-Yin deficiency pattern of dry eye, a relatively consistent trend was found, except for purine metabolism, in five specific pathways: lysine degradation, ovarian steroidogenesis, cholesterol metabolism, pyrimidine metabolism, and bile secretion, where metabolites mainly showed an upward trend, indicating a potentially significant increase in these metabolic pathways in the Qi-Yin deficiency pattern of dry eye (P < 0.05).
TCM theory holds that dry eye is caused by both internal and external factors, such as emotional distress, improper diet, excessive fatigue, and prolonged visual strain, causing an imbalance of Yin and Yang, disharmony of Qi and blood, and dysfunction of the internal organs. These internal and external factors affect the normal production and metabolism of tears, thereby causing dry eye. Modern TCM, based on different causes and symptoms, divides it into different types of treatment. Among them, patients with heat stagnation in liver meridian pattern of dry eye may demonstrate changes in the quality of tears, such as increased viscosity and poor excretion. At this time, metabolites in tears may show an increase in inflammatory markers and cytokines, causing metabolic disorders [10]. Patients with a Qi-Yin deficiency pattern of dry eye may have insufficient tear secretion. Meanwhile, the antioxidant substances in tears decrease, causing the eyes more susceptible to damage from free radicals [11]. Dry eye is a multifactorial disease of tears and the ocular surface. The key to treating dry eye is to address the main pathogenic mechanisms and resolve secondary mechanisms [12]. By analyzing the metabolites in the tears of patients with different pattern, results showed that they can play a beneficial role in more accurately determining the patient’s type via TCM, thereby formulating personalized treatment plans. At the same time, it is conducive to deeply understanding the pathogenesis of dry eye, which is beneficial for the development of related drugs.
In this study, compared with patients with the heat stagnation in liver meridian pattern of dry eye, patients with the Qi-Yin deficiency pattern of dry eye showed more changes in tear metabolites, with seven related metabolic pathways: lysine degradation, ovarian steroidogenesis, cholesterol metabolism, pyrimidine metabolism, bile secretion, purine metabolism, and caffeine metabolism pathways. Abnormal lysine degradation and cholesterol metabolism disorders are closely correlated with decreased tear secretion. Lysine is an amino acid, and its metabolites may cause oxidative stress, damaging the lacrimal and meibomian glands, thereby causing insufficient tear secretion and then symptoms of dryness and lack of luster in the eyes [13]. Cholesterol, an important component of meibomian gland secretions, helps maintain the lubrication and health of the ocular surface. This study found that the disorder of cholesterol secretion and excretion indicates a poor lubrication state of the ocular surface, which is similar to the clinical manifestations of dry eye. Simultaneously, ovarian steroidogenesis requires cholesterol as a precursor substance, and metabolic disorders may affect the supply and conversion of cholesterol, affecting the generation of ovarian steroids consequently [14]. The interaction between the two can significantly affect the lubrication and health of the ocular surface.
In addition, bile acids, as part of tears, maintain the lubrication and protection of the ocular surface. Bile plays a role in fat metabolism, and fat is an important component of cell membrane structure and function [15]. Insufficient bile secretion in the Qi-Yin deficiency pattern may lead to malnutrition of ocular tissues, affecting the clarity of vision. Moreover, abnormalities in the purine and caffeine metabolism may result in an insufficient cellular energy supply, which have an impact on the function of ocular tissues. Abnormalities in the purine and caffeine metabolism involve cellular energy metabolism disorders, influencing the normal function of the lacrimal glands, causing discomfort in the eyes, photophobia, and other symptoms. Dry eye symptoms, especially after prolonged use of the eyes, may worsen, which is related to insufficient cellular energy supply and inflammatory reactions. Abnormalities in the pyrimidine, purine, and caffeine metabolism are related to the presence of mitochondrial dysfunction in dry eye patients [16]. Mitochondria serves as the main site of energy production within cells. Abnormalities in the metabolism of pyrimidine, purine, and caffeine can impair mitochondrial function, which in turn affects cellular energy supply. This impairment, including the energy needs of the lacrimal and meibomian glands, can exacerbate the occurrence and development of dry eye.
In summary, abnormalities in the metabolism of pyrimidine, purine, and caffeine reduce the energy supply of the human body, leading to Qi deficiency. Lysine degradation, ovarian steroidogenesis, cholesterol metabolism, and bile secretion affect the secretion of human Yin fluids, which demonstrates Yin deficiency. Therefore, the abnormalities in these seven metabolic pathways jointly affect the Qi-Yin deficiency pattern of dry eye.
The heat stagnation in liver meridian pattern of dry eye is a classification in the syndrome differentiation of TCM. TCM theory holds that it is related to the dysfunction of liver function, leading to the stagnation of Qi and the generation of internal heat, causing several eye symptoms, such as dry eyes, red eyes, blurred vision, and emotional fluctuations. Heat stagnation refers to the accumulation of Qi stagnation and heat evil in the body, leading to liver Qi discomfort and poor Qi movement. Heat stagnation in liver meridian is linked to psychological states such as emotional depression, mental tension, and anger, which are associated with the regulation of hormones and other biologically active substance levels, potentially influencing the endocrine system and metabolic status.
In this study, the caffeine and purine metabolism pathways were not only significantly enriched in the heat stagnation in liver meridian but also the Qi-Yin deficiency patterns of dry eye, indicating that they may play an important part in the common pathological process of dry eye. Caffeine and purine metabolism belong to one of the energy metabolisms, and their occurrence and development are strongly correlated with free radicals [17]. Caffeine metabolism involves the degradation and clearance process of caffeine, and its metabolites may be closely related to the generation of free radicals, affecting the cellular oxidative stress response as a result. Oxidative stress is a key pathological feature of dry eye, and excessive free radicals can cause damage and inflammatory reactions in ocular tissues. Purine metabolism is involved in the synthesis and utilization of cellular energy, such as the generation of adenosine triphosphate (ATP) and guanosine triphosphate (GTP). Its abnormalities may lead to insufficient cellular energy supply, especially for the high metabolic demand of the lacrimal and meibomian glands, thus exacerbating dry eye symptoms [18]. Unlike the Qi-Yin deficiency pattern of dry eye, an important metabolic pathway in patients with the heat stagnation in liver meridian pattern of dry eye is the biosynthesis pathway of valine, leucine, and isoleucine. Valine, leucine, and isoleucine are all branched-chain amino acids, which are key amino acids that play an important role in muscle protein synthesis, immune function regulation, and liver metabolism. Abnormalities in the metabolism of branched-chain amino acids are often related to liver dysfunction, which may result in changes in mood and mental state, changes that are similar to the “heat stagnation” described by TCM [19].
Furthermore, long-term nutritional imbalance, including abnormalities in branched-chain amino acids, may cause metabolic disorders in the body, which can affect a person’s physical and mental health in various forms (e.g., hormonal imbalance), corresponding to the “liver depression” described by TCM [20]. The Treatise of the True Doctrine of the Golden Coffer in the Inner Cannon of Haungdi on Plain Questions (Huang Di Nei Jing · Su Wen,《黄帝内经·素问》) recorded that “the liver opens into the eyes.” It is believed that a special intrinsic connection between the liver and the eyes exists; thus diseases of the liver are often thought to influence the function of the eyes. Studies have proposed that the liver and eyes share characteristics of co-damage, co-repair, co-material basis, and co-mechanism of action [21]. From the perspective of metabolomics, this further proves the rationality of the classification of dry eye due to stagnant heat in the liver channel.
This study still has some limitations. First, the current sample size is small as an exploratory experiment, which may affect the generalizability of the results. Future research is warranted to determine the minimum required sample size based on the results of this study, using sample size calculation formulas to strengthen the reliability of the findings. Second, the diagnostic criteria for TCM syndromes mainly rely on subjective descriptions, which may impact the reproducibility of the results. Quantitative assessment methods, such as scoring systems or questionnaires, should be introduced and unified diagnostic criteria and procedures should be established in subsequent large-scale studies to reduce the interference of subjective factors. Moreover, the present study did not provide details of the relevant clinical and laboratory testing indicators, which limits the comprehensiveness of dry eye diagnoses. Finally, key metabolites and functional clusters still require further validation. Despite these shortcomings, this research provides a preliminary reference for future large-scale experiments and lays the foundation for in-depth exploration of the metabolic characteristics of dry eye.
The clinical metabolism of dry eye patients with Qi-Yin deficiency and heat stagnation in liver meridian patterns has its own characteristics and is significantly varied. Among them, purine and caffeine metabolism pathways are common metabolic characteristics of both patterns of dry eye. dIMP and 2-(formamido)-N1-(5-phospho-D-ribosyl) acetamidine can be used as biomarkers. In the Qi-Yin deficiency pattern, the significant increase of metabolic pathways, such as lysine degradation, ovarian steroidogenesis, cholesterol metabolism, pyrimidine metabolism, and bile secretion, remains the main feature. The dry eye of the heat stagnation in liver meridian pattern is featured with the inhibition of the valine, leucine, and isoleucine biosynthesis pathway. The above results prove the rationality of the TCM syndrome differentiation classification and are of crucial reference for the exploration of the pathogenesis of dry eye and the development of related drugs.
National Natural Science Foundation of China Project (82305037), Guiding Project for Innovative Clinical Medical Technology in Hunan Province (2021SK50809), and Scientific Research Project of Hunan Administration of Traditional Chinese Medicine (D2022053).
Competing Interests: The authors declare no conflict of interest
| [1] |
INOMATA T, IWAGAMI M, HIRATSUKA Y, et al. Maximum blink interval is associated with tear film breakup time: a new simple, screening test for dry eye disease. Scientific Reports, 2018, 8(1): 13443. doi: 10.1038/s41598-018-31814-7
|
| [2] |
LIU ZG, WANG H. Chinese Consensus on the Treatment of Dry Eye Disease (2020). Chinese Journal of Ophthalmology, 2020, 56(12): 907–913 doi: 10.3760/cma.j.cn112142-20200925-00618
|
| [3] |
LEMP MA, BAUDOUIN C, BAUM J, et al. The Definition and Classification of Dry Eye Disease: Report of the Definition and Classification Subcommittee of the International Dry Eye WorkShop (2007). Ocular Surface, 2007, 5(2): 75-92.
|
| [4] |
PENG QH, XIE LK, WANG YL, et al. International Clinical Practice Guideline for Dry Eye (2021-12-14). World Chinese Medicine, 2022, 17(16): 2235–2239, 2244.
|
| [5] |
WANG YF, SONG L. A brief discussion on the application of “Xuanfu theory” in the syndrome differentiation of dry eye. Chinese Journal of Traditional Chinese Medicine, 2017, 32(3): 1132–1134. doi: CNKI:SUN:BXYY.0.2017-03-068
|
| [6] |
VEHOF J, HYSI PG, HAMMOND CJ. A metabolome-wide study of dry eye disease reveals serum androgens as biomarkers. Ophthalmology, 2017, 124(4): 505–511. doi: 10.1016/j.ophtha.2016.12.011
|
| [7] |
PIERAGOSTINO D, AGNIFILI L, CICALINI I, et al. Tear film steroid profiling in dry eye disease by liquid chromatography tandem mass spectrometry. International Journal of Molecular Sciences, 2017, 18(7): 1349. doi: 10.3390/ijms18071349
|
| [8] |
PENG QH, LI ZJ, XIE XJ, et al. Traditional Chinese medicine and ophthalmology. Shanghai: Shanghai Science and Technology Press, 2019.
|
| [9] |
LIU P, JIANG PF, LIANG H, et al. Proteomic study of tear fluid in patients with dry eye due to liver meridian heat stagnation. Chinese Journal of Traditional Chinese Medicine, 2022, 37(5): 2712–2717
|
| [10] |
LI CW, ZHOU SK, LIU J, et al. Clinical study on the treatment of dry eye with liver heat stagnation syndrome by Chrysanthemum and Lotus fumigation eye method. Chinese Journal of Ophthalmology in Traditional Chinese Medicine, 2023, 33(8): 727–731. doi: 10.13444/j.cnki.zgzyykzz.2023.08.006
|
| [11] |
LAI JP, HUANG QZ, CHI MQ, et al. The effect of modified Zengye Decoction combined with self-formulated atomization solution on the treatment of dry eye syndrome with deficiency of both Qi and Yin and the indicators of ocular surface function. Inner Mongolia Traditional Chinese Medicine, 2023, 42(12): 26–28. doi: 10.16040/j.cnki.cn15-1101.2023.12.003
|
| [12] |
SHAO Y, CHEN LJ, ZHOU J, et al. Diagnostic Evaluation and Treatment Guidelines for Dry Eye-Interpretation of the 2021 Expert Consensus. Recent Advances in Ophthalmology, 2022, 42(10): 757–762
|
| [13] |
SCHLEGEL I, DE GOÜYON MATIGNON DE PONTOURADE CMF, LINCKE JB, et al. The human ocular surface microbiome and its associations with the tear proteome in dry eye disease. International Journal of Molecular Sciences, 2023, 24(18): 14091. doi: 10.3390/ijms241814091
|
| [14] |
ASFUROĞLU Y, KAN Ö, ASFUROĞLU M, et al. Association between dry eye and polycystic ovary syndrome: subclinical inflammation may be part of the process. Eye & Contact Lens, 2021, 47(1): 27–31. doi: 10.1097/ICL.0000000000000716
|
| [15] |
CAMPAGNOLI LIM, VARESI A, BARBIERI A, et al. Targeting the gut-eye axis: an emerging strategy to face ocular diseases. International Journal of Molecular Sciences, 2023, 24(17): 13338. doi: 10.3390/ijms241713338
|
| [16] |
QU ML, WAN L, DONG MC, et al. Hyperglycemia-induced severe mitochondrial bioenergetic deficit of lacrimal gland contributes to the early onset of dry eye in diabetic mice. Free Radical Biology & Medicine, 2021, 166: 313–323. doi: 10.1016/j.freeradbiomed.2021.02.036
|
| [17] |
STEFANELLO N, SPANEVELLO RM, PASSAMONTI S, et al. Coffee, caffeine, chlorogenic acid, and the purinergic system. Food and Chemical Toxicology, 2019, 123: 298–313. doi: 10.1016/j.fct.2018.10.005
|
| [18] |
NAVEL V, SAPIN V, HENRIOUX F, et al. Oxidative and antioxidative stress markers in dry eye disease: a systematic review and meta-analysis. Acta Ophthalmologica, 2022, 100(1): 45–57. doi: 10.1111/aos.14892
|
| [19] |
CUOMO, CAPPARELLI R, IANNELLI A, et al. Role of branched-chain amino acid metabolism in type 2 diabetes, obesity, cardiovascular disease and non-alcoholic fatty liver disease. International Journal of Molecular Sciences, 2022, 23(8): 4325. doi: 10.3390/ijms23084325
|
| [20] |
NEINAST M, MURASHIGE D, ARANY Z. Branched chain amino acids. Annual Review of Physiology, 2019, 81: 139–164. doi: 10.1146/annurev-physiol-020518-114455
|
| [21] |
XIONG SH, YU JH, SUN M, et al. "The liver opens into the eyes" under the enlightenment of the "four common characteristics" of liver and eye and research ideas. Chinese Journal of Experimental Formulas, 2023, 29(17): 185–194. doi: 10.13422/j.cnki.syfjx.20230841
|